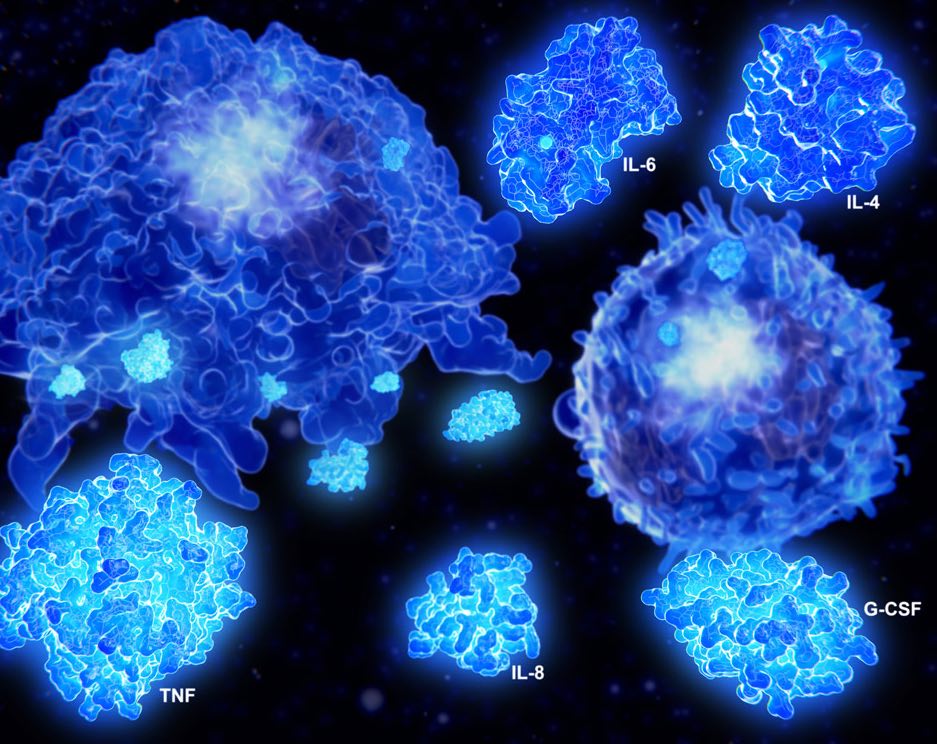
Cytokines are small molecules important in cell signaling. Much like hormones, they are secreted by various cells to act as chemical messengers, affecting the behavior of other cells.
Cytokines are regulators of adaptive and innate immunity, controlling the intensity and duration of immune responses. These molecules help abnormal cells die while prolonging the life of healthy cells.
Immune cells aim to eliminate toxins and other foreign substances in the body, known as antigens. Upon binding to an antigen, the cell secretes cytokines that deliver signals to induce an immune response. So begins a cascade of intracellular signaling that alters cell functions of the releasing cell itself, or neighboring cells.
There are a multitude of different cytokines with various functions, and each cytokine has a matching cell-surface receptor. Some cytokines are antagonistic to one another, in that one cytokine stimulates a particular defense function while another cytokine inhibits that function. Other cytokines work synergistically, having a greater effect in combination than either would by themselves.
Cytokines and cancer treatment
Cytokines can be used to treat cancer and reduce the side effects of cancer treatment by promoting the growth of healthy blood vessels. Some immunotherapies use cytokines to help immune cells grow, multiply more quickly, or attack cancer cells.
Below, we discuss three different types of cytokines and their potential to treat cancer.
Interferons (INFs)
Interferons are named for their ability to “interfere” with viral replication. They are the body’s fastest-produced and most important defense against viruses.
In addition to activating immune cells, interferons can also fight infections, halt cell division, and promote or inhibit the differentiation of cells. Importantly, interferons can regulate antigen expression in a Major Histocompatibility Complex (MHC).
An MHC complex is a gene conglomerate in charge of presenting the antigen to a type of immune cell called a T-cell. This modulation and presentation is vital to proper immune function as it allows immune cells to differentiate between cells normally found in the body and foreign invaders, and enables an immune response specifically designed for the infectious agent.
One type of interferon, INF-alpha, can enhance the immune response by causing some white cells, such as natural killer (NK) cells and dendritic cells, to become active. Activating NK cells means that they are primed and ready to kill infected body cells. This ability to directly kill is often referred to as cytotoxicity. Therefore, activation of NK cells allows them to be cytotoxic or toxic to cells.
Interleukins (ILs)
Interleukins are small effector molecules with a myriad of functions including helping with cell development and immune response regulation.
In addition to activating immune cells, interferons can also fight infections, halt cell division, and promote or inhibit the differentiation of cells. Importantly, interferons can regulate antigen expression in a Major Histocompatibility Complex (MHC).
An MHC complex is a gene conglomerate in charge of presenting the antigen to a type of immune cell called a T-cell. This modulation and presentation is vital to proper immune function as it allows immune cells to differentiate between cells normally found in the body and foreign invaders, and enables an immune response specifically designed for the infectious agent.
One type of interferon, INF-alpha, can enhance the immune response by causing some white cells, such as natural killer (NK) cells and dendritic cells, to become active. Activating NK cells means that they are primed and ready to kill infected body cells. This ability to directly kill is often referred to as cytotoxicity. Therefore, activation of NK cells allows them to be cytotoxic or toxic to cells.
Granulocyte-colony stimulating factor (G-CSF) and Granulocyte/Macrophage-colony stimulating factor (GM-CSF)
These cytokines boost the number of circulating white cells, which reduces the risk of infection and enhances the immune response against cancer.
Granulocyte-colony stimulating factor (G-CSF)
G-CSF functions as both a cytokine and a hormone, stimulating the bone marrow to produce stem cells and a type of white blood cell known as a granulocyte. Continual stimulation of G-CSF allows for proliferation, differentiation, and function of the most abundant type of granulocyte, called neutrophils.
There are a variety of clinical uses for G-CSF being explored. For example, G-CSF has been used to help chemotherapy patients regain neutrophil cell count, thus allowing patients to recover much faster.
Granulocyte/Macrophage-colony stimulating factor (GM-CSF)
GM-CSF stimulates the production of more immune cell types than G-CSF, especially a type of granulocyte called an eosinophil, and a type of monocyte known as a macrophage. Activation of a small number of macrophages can quickly lead to an increase in their numbers, which is crucial for fighting infection. Another essential function of GM-CSF is the differentiation of dendritic cells, which are the most potent antigen-presenting cells of the immune system.
A number of cancer immunotherapies have been developed using GM-CSF to enhance antigen-specific immune responses when used in combination with specific vaccine antigens. Clinical trials of such therapies have been shown to improve the survival of patients with various types of cancer.